Introduction
Assignment
With an ageing Nordic population, the number of people with dementia keeps growing. An increasing number of people at risk of developing dementia poses a major challenge to individuals and the society at large. The Nordic Council of Ministers for Health and Social Affairs has therefore highlighted the need to map policies and practices on dementia prevention in the Nordic countries. In 2023–2024, the Nordic Welfare Centre was assigned by the Nordic Council of Ministers to manage the project on dementia prevention in the Nordic countries. The Norwegian National Centre for Ageing and Health committed as a core partner in this project and undertook the task to map and compile the report. This compilation of the status and development in the field of dementia and prevention provides important knowledge of the Nordic efforts to design measures that promote brain health, preserve cognitive capacity, and, to an extent, delay or prevent symptoms of dementia.
Purpose
The purpose is to explore dementia prevention in the Nordic countries, give examples of policies and practices, and to review these measures in relation to current evidence on dementia prevention.
The report seeks to answer the following questions:
- What does dementia prevention look like in the Nordic countries and Åland Islands, and are prevention efforts put into practice in line with the current evidence?
- What are the barriers and opportunities for the Nordic countries to include a preventative perspective on dementia?
- What is the role of strategic governance and organisational aspects in dementia prevention?
- How can prevention of dementia delineate or interact with existing public strategies for the prevention of NCDs such as heart disease or diabetes?
Dementia diseases
Dementia is a condition characterised by changes in cognition and behaviour to such an extent that it affects the ability to cope with daily life. The criteria for dementia are listed in the international classification system of diseases ICD-10 (World Health Organization [WHO], 2004). Dementia can be caused by several different diseases, of which Alzheimer’s disease (AD) is the most common. Other common types of dementia are vascular dementia, Lewy body dementias, and frontotemporal dementia. Mild cognitive impairment (MCI) can be a precursor to dementia with changes in previous levels of cognitive function which do not substantially affect activities of daily living.
Worldwide, 55 million people are living with dementia, and 75 million are estimated to live with dementia in 2030 (Alzheimer’s Disease International, 2021). Unfortunately, there are no fully comparable Nordic statistics on dementia prevalence or incidence, due to lack of comparable data collecting methods in the Nordic countries, but it is estimated that the number of people with dementia will more than double by 2050 in Norway (Gjora et al., 2021), and the situation is likely the same for the entire Nordic region. Prevalence and incidence are defined in fact box 1. The picture is further clarified by two examples, one on the estimated prevalence of dementia in Norway and the other by incidence of dementia in Finland.
Fact box 1. Prevalence and incidence of dementia.
Prevalence: Prevalence is the proportion of a population who have dementia in a given time (National Institute of Mental Health, 2024).
Incidence: Incidence is a measure of the number of new cases of dementia that develop in a population in a specific time period (National Institute of Mental Health, 2024).
|
Importance of dementia prevention
Dementia is a key challenge globally (Alzheimer’s Disease International, 2024; WHO, 2019). The Nordic countries are no exception. The risk of developing dementia increases with age, and the Nordic population is ageing rapidly.
The societal costs of dementia are high both in Europe and in the Nordic countries (Jonsson et al., 2023). The increased proportion of older adults in the society drives the increase in health spending, shows a study from Norway on future disease-specific health spending (Kinge, 2023). The total societal costs of dementia in Sweden are calculated to total SEK 81.6 billion based on various population studies (Karolinska Institutet, 2023). The ageing population and increased prevalence of preventable NCDs is a challenge to the healthcare systems in the Nordic countries and has fuelled political interest in health promotion and prevention.
While dementia has been considered to be beyond our control, an emerging body of evidence shows that optimal environmental and lifestyle factors support cognitive functions and can protect against dementia. Thus, dementia prevention has lately become an important topic on the Nordic public health agenda.
Research and evidence
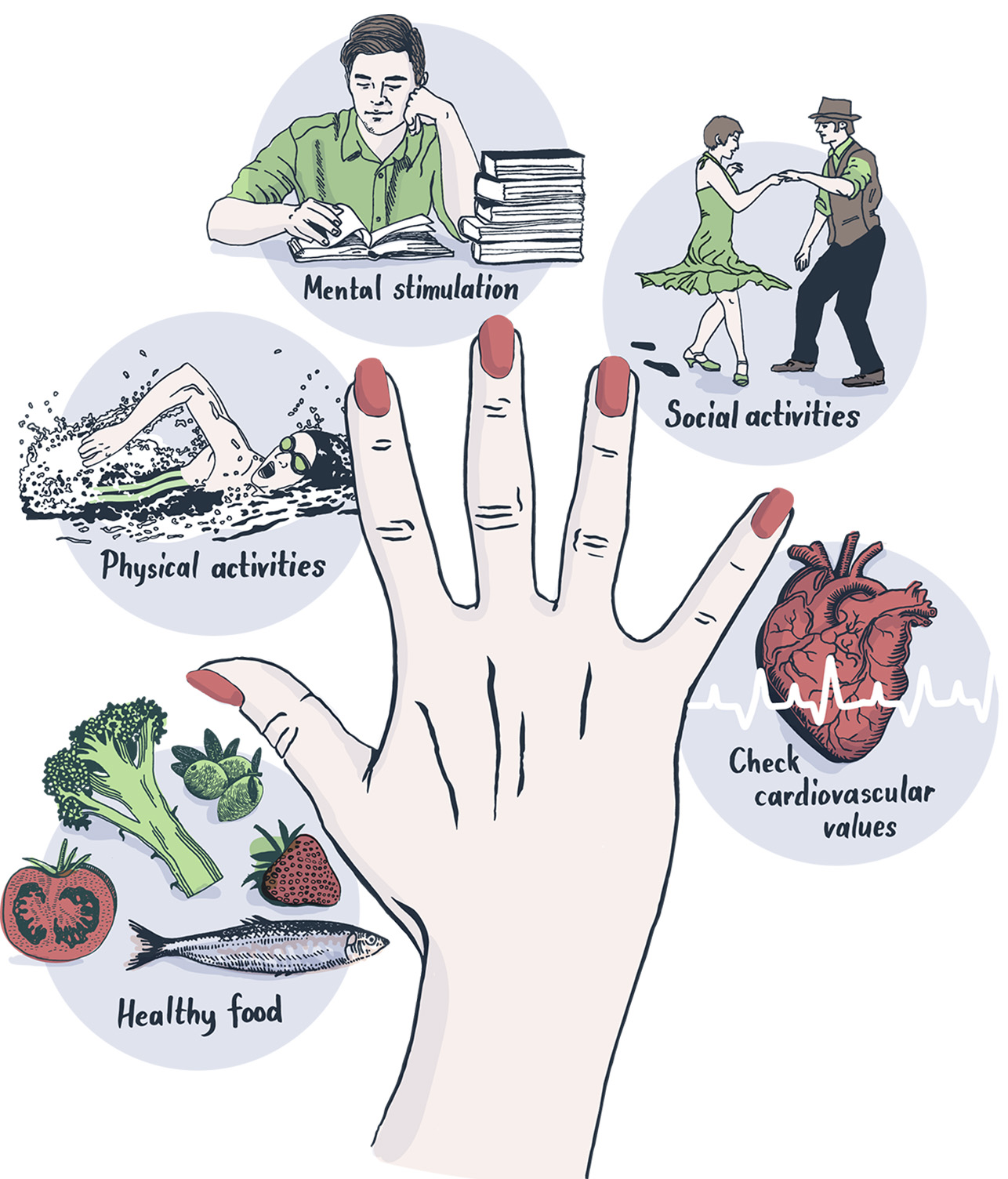
Since 2009, several studies have showed a falling incidence of dementia in the USA and the European countries (Middleton & Yaffe, 2009; Wolters et al., 2020). These results have inspired researchers to investigate which factors have influenced the decline and if there are opportunities for prevention. In 2015, the Finnish Geriatric Intervention Study to Prevent Cognitive Impairment and Disability study (FINGER), was the first published randomised control trial to show that modification of a set of lifestyle factors in older adults can slow down cognitive decline in later life (Ngandu et al., 2015). The FINGER study has since expanded to a large international network from over 62 countries, called the World Wide Finger Network (World Wide Finger, 2024). Figure 1 shows the FINGER model based on a combination of five healthy lifestyle measures: healthy food, physical activity, cognitive challenges, social stimulation in group activities, and control of vascular risk factors.
Figure 1. The FINGER model. Illustrations: Martina Krona in Kivipelto & Hellénius (2022).
The Lancet Commission on Dementia Prevention, Intervention and Care is a platform of international group of experts, who – led by a team at University College London – made a comprehensive literature review and produced recommendations for practice on Dementia prevention, intervention, and care. Since 2017, when the commission published the first evidence-based report on prevention and intervention in dementia care, the prevention of dementia has gained even more focus in research (Livingston et al., 2017). The 2017 report described nine modifiable risk and protective factors that have different significance in different phases of life. The research and volume of scientific articles in the field of dementia prevention has increased remarkably. Figure 2 illustrates the development in research over time based on the number of hits in PubMed on research articles in 1990–2024.
Figure 2. Timeline of results per year in PubMed with search query “Dementia prevention, 1990–2023”.
The World Health Organization declared dementia as a public health priority in 2019 and provided evidence-based recommendations on lifestyle behaviours and interventions to delay or prevent cognitive decline and dementia (WHO, 2019). The Lancet Commission on Dementia Prevention, Intervention and Care published a follow-up publication in 2020, urging nations, stakeholders, and individuals to be ambitious about dementia prevention (Livingston et al., 2020).
Figure 3. Timeline of the development in the field of dementia prevention during the last 10– 15 years. (Figure designed by the Norwegian National Centre for Ageing and Health, Linn Lundsvoll/Grete Kjelvik).
Risk factors for dementia
Nine modifiable risk factors for dementia were identified by the 2017 Lancet Commission on Dementia Prevention, Intervention and Care in 2017. Those were low educational attainment, hearing loss, hypertension, obesity, tobacco smoking, depression, social isolation, physical inactivity, and diabetes (Livingston et al., 2017). In 2020, three more factors were added: air pollution, alcohol, and brain injury (Livingston et al., 2020). Figure 4 illustrates the 12 modifiable risk factors for dementia.
Figure 4. 12 modifiable risk factors for dementia. (Made by Martin Lundsvoll/ Grete Kjelvik, illustrations by Headspin AS).

The 2020 Lancet Commission on Dementia Prevention, Intervention and Care estimated that 40 percent of the dementia cases could be prevented or delayed globally by targeting these 12 modifiable risk factors in a life-course perspective from the very young to older adults (Livingston et al., 2020). Healthy lifestyle changes, less air pollution and monitoring of hypertension and hearing loss, can have a significant societal impact on the future burden of disease caused by dementia and other diseases.
Since the non-modifiable risk factors age, sex, and genetics cannot be altered, it’s important to recognize the power in the modifiable risk factors listed by Livingston et al (2020). Health-enhancing factors can mitigate the risk of dementia also in people with high genetic vulnerability. Risk accumulates throughout the life course, and health behaviours may need to be improved or altered 30 or 40 years prior to the onset of the disease. Consequently, the primary prevention of dementia is as challenging as for other NCDs. The most effective prevention is a health-promoting lifestyle and society from early childhood. Figure 5 shows a life-course model based on evidence of potentially modifiable risk factors for dementia.
“It’s never too early nor too late in the life course for dementia prevention.”
Livingston et al. (2020)
Figure 5. Population-attributable fraction of potentially modifiable risk factors for dementia. Copyright: Livingston et al., 2020. Dementia prevention, intervention, and care. 
Intellectual disability
People with intellectual disabilities belong to a high-risk group of developing dementia (Strydom et al., 2013). People with Down syndrome have an even higher risk of developing dementia due to the non-modifiable factor of genetics (Fortea et al., 2021). Also, this group often has lifestyle risk factors to dementia: according to McCarron and colleagues (2017), the risk of dementia for people with Down syndrome is 23% at age 50, 45% at age 55 and 85% at age 65. An estimated six million people worldwide have Down syndrome (Ballard et al., 2016), making them likely the largest single population group in the world at a heightened risk of dementia. In their report of autumn 2023, Alzheimer’s Disease International calls for a greater focus on the prevention of dementia among people with Down syndrome (Long et al., 2023).
Given that people with intellectual disabilities often have lifestyle risk factors for dementia, a preventive approach is needed. The potentially modifiable factors in this group include lack of access to education and employment, higher rates of sleep apnea, vision and hearing impairments, diabetes, and obesity (Aslam et al., 2022). For people with Down syndrome, a large European study shows that sleep problems, mental health problems, and several co-occurring conditions were associated with early onset of dementia in younger ages (Larsen et al., 2024). Individuals with intellectual disabilities, both with and without Down syndrome, are often overweight, have a poor diet and get little physical activity, and they often experience loneliness.
Definitions of prevention
Prevention is an ambiguous and positively charged term for attempts to eliminate or limit an undesirable development. Prevention of a disease can be defined as three levels: primary, secondary and tertiary prevention (Last, 2001; Szklo, 2007).
Figure 6. Prevention of dementia. (The Norwegian National Centre for Ageing and Health, Linn Lundsvoll and Grete Kjelvik)
This section clarifies the conceptual understanding of the different levels of prevention.
1. Primary preventative measures
Primary prevention measures aim to prevent health impairment in healthy and vulnerable people/people at risk. Primary prevention includes measures that prevent disease before the disease process begins (Last, 2001). This is done by preventing exposure to hazards that cause the disease, influencing unhealthy or unsafe behaviours that can lead to disease, and increasing resistance to disease should exposure occur (Den norske regjeringen, 2011). Primary preventive measures against dementia risk and for maintaining good brain health can be implemented at the individual and population levels. Health promotion is the process of enabling people to increase control over and to improve their health (Nutbeam, 1986).
2. Secondary preventative measures
Secondary prevention includes measures that enhance early diagnosis and prompt treatment of a disease and to offer symptom relief. Secondary prevention also seeks to prevent the onset of further symptoms or disease. This is done by detecting and treating disease as soon as possible to slow down its progress, encouraging personal strategies to prevent disease-related complications and recurrence, and implementing programmes to return people to their original state of health and function to prevent long-term problems.
3. Tertiary preventative measures
Tertiary prevention aims to reduce the effects of the disease once established in an individual. Tertiary prevention aims to mitigate the impact of an ongoing disease that has lasting effects, such as dementia. This is done by helping people manage long-term often complex health problems such as chronic disease and permanent impairments to improve their ability to function, their quality of life, and life expectancy as much as possible (Den norske regjeringen, 2011).
The focus in this report is on primary prevention of dementia. Secondary and tertiary prevention will be touched upon more briefly.
Prevention: Population level vs individual level
Preventive measures against dementia risk and for maintaining good brain health can be implemented at the individual and population levels.
An individual-level approach targets people’s lifestyle-related risk factors for dementia development and encourages adoption of healthier behaviours. Adopting a healthy lifestyle requires conscious behavioural change. Examples of preventive behavioural changes among high-risk individuals include increasing the level of physical exercise, quitting smoking, and undertaking cognitive training, in addition to dietary advice to help normalise their weight and reduce obesity (WHO, 2022).
Population-level prevention targets the risk profile of communities or the entire population by changing societal conditions and is characterised by unconscious behavioural change (Walsh, 2023). Examples of population-level prevention measures are national screening-programmes, awareness campaigns, public health guidance, and promoting healthy ageing through plans and strategies (WHO, 2022). Population-based approaches require engagement from a broad group ranging from stakeholders in local government to politicians at the national level. An unequal distribution of social determinants of health conditions in which people are born, grow up, live, work, and age are also important factors to focus on in regulating and legalising efforts at population level.
Table 1. Examples of prevention policies in relation to risk factors for dementia according to an individual or population approach (Walsh, 2022).
Risk factor | High-risk individual prevention (Conscious behaviour change) | Whole population prevention (Unconscious behaviour change) |
Obesity and physical inactivity |
|
|
Poor diet |
|
|
High blood pressure |
|
|
Smoking |
|
|
Low education and lack of cognitive stimulation |
|
|
Social isolation and loneliness |
|
|
Examples of prevention policies against risk factors for dementia, according to individual or population approach. Reused from Walsh et al.2022 under a CC BY 4.0. copyright agreement. | ||
Prevention of dementia and other non-communicable diseases
Dementia is a non-communicable, chronic, and serious disease. Many of the risk and protective factors for dementia are identical with those for other NCDs (WHO, 2013). At the same time, dementia is defined to varying degrees as an NCD in strategic documents. The European Commission defines dementia as a type of NCD (European Commission, 2024), while the WHO does not (WHO, 2023). Based on an unclear classification, there are different approaches to prevention efforts in relation to dementia. The implementation of preventative measures against dementia might be combined in preventative programmes to reduce the risk of NCD, either primary prevention with a perspective on broad measures at population level or a risk-group perspective with measures at group and individual level.
The European joint action Prevent NCDs, coordinated by the Norwegian Institute of Public Health and the Norwegian Directorate of Health strives to improve the system of monitoring NCDs and their common risk factors. Joint Action Prevent NCDs started on 1 January 2024 and is designed to improve the planning and implementation of prevention policies and activities at national, regional, and local levels. With 10 work packages, the European project will last at least four years. The project addresses health determinants common to cancer and NCDs, and examples of work packages are Regulation and taxation and Identify individuals at risk (European Union, n.d.). Task 1 is designed to prepare general and country-specific reports for decision- and policymakers based on real-world data on prevention strategies for dementia and stroke. Enhancing cross-national collaboration fosters a sense of unity and shared responsibility in addressing global health challenges.
The WHO global action plan on the public health response to dementia 2017–2025 includes a set of actions to deliver on the vision of a world in which dementia is prevented. The third action area, dementia risk reduction, states that there is growing evidence to suggest an interrelationship between dementia on the one hand and noncommunicable disease and lifestyle-related risk factors on the other (WHO, 2019).
“We need to do everything we can to reduce our risk of dementia. The scientific evidence gathered for these Guidelines confirms what we have suspected for some time, that what is good for our heart, is also good for our brain.”
Director-General of WHO, Dr Tedros Adhanom Ghebreyesus (2019)